Introduction: There is growing recognition of germline cancer predisposition syndromes (CPS) that increase risk of hematologic malignancies including leukemias, lymphomas, bone marrow failure syndromes and myeloproliferative diseases. Somatic (tumor) testing can identify potential germline variants based on multiple factors including variant allele fraction, sequence characteristics, and other findings; however, subsequent germline testing is required to characterize the lesion. Paired tumor and germline testing (T/N testing) is more accurate to diagnose CPS and may mitigate loss to follow-up, reduce time to CPS diagnosis, and possibly alleviate unnecessary anxiety due to suspected but ultimately disproved germline conditions. Previously, our center performed tumor-only diagnostic testing for patients with newly diagnosed hematologic malignancies. In 2020 we transitioned to paired T/N testing for all new hematologic malignancy diagnoses with patient/caregiver consent. Here we report the frequency of CPS diagnoses suggested by tumor-only testing and subsequently confirmed with germline testing, as well as CPS diagnoses identified from the outset by T/N testing.
Methods: Data was automatically abstracted from the Children's Hospital of Philadelphia (CHOP) Diagnostic Genomics Database (FileMaker and Nexus) for 1057 pediatric, adolescent, and young adult patients who underwent testing with the CHOP Comprehensive Hematologic Malignancy panel between 2016 and 2023. This panel interrogates 117 genes for single nucleotide variants, insertions, deletions, and copy number variants. Of those tested, 932 patients underwent tumor-only testing, and 125 patients underwent paired T/N testing. Characteristics of patients with possible pre-established genetic syndromes (e.g. Trisomy 21) were cross-checked via manual chart review.
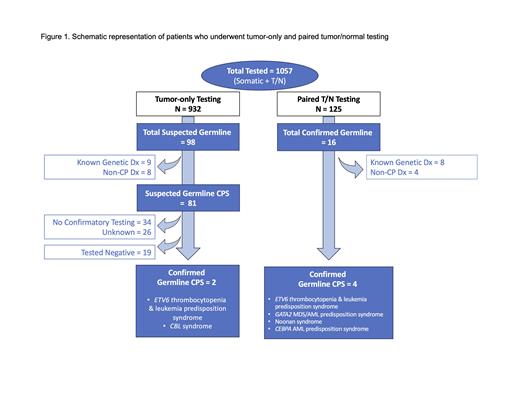
Results: Schematic representation of patient testing is summarized in Figure 1. Among 932 patients who underwent tumor-only testing, 98 were identified to have potential or previously established germline pathogenic variants. Of these, 9 had known genetic syndromes and 8 had non-cancer related genetic diagnoses (e.g. Usher syndrome). Of the 81 patients with a suspected CPS, 26 were referred from an outside hospital with unavailable follow-up data. Among suspected germline patients from our center (n=55), 34 (62%) did not undergo confirmatory testing. Of the 21 (38%) who underwent confirmatory testing, 2 (10%) were diagnosed with a CPS. For patients with T/N testing, 16 of 125 (7%) were identified to have germline conditions; 8 were pre-established diagnoses and 4 were non-cancer related genetic diagnoses. Thus, 4 (3%) of patients with T/N testing were newly diagnosed with a CPS. New CPS diagnoses included: ETV6 thrombocytopenia and leukemia predisposition syndrome, CBL syndrome, GATA2 MDS/AML predisposition syndrome, Noonan syndrome, and CEBPA AML predisposition syndrome.
Conclusion: At our center, 62% of patients with suspected germline conditions on tumor-only testing had no follow up testing documented in the available medical record. These data suggest that paired T/N testing at the time of hematologic malignancy diagnosis assists in mitigating loss-to-follow up for patients with possible CPS. Additionally, T/N testing may streamline result interpretation, reduce time to diagnosis, aid in treatment decisions, and guide cascade testing for potentially affected family members. When possible, genetic testing decisions and results should be discussed with a trained genetic counselor. Over time, increasing utilization of paired T/N testing may also enhance understanding of CPS-associated genes that increase risk of hematologic malignancies.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal